Q – Justin Starbird: Something that’s important to consider from all of the clients that we work with is, what are the options in optical devices, and how do clients evaluate hybrid systems, versus disposable versus reusable. As well as some of the checklist, if you will, that folks should be evaluating, and what comes out on the other side once we have a completed project.
A – Benjamin Gray: It’s really quite a large subject. One of the first things that we find in evaluation of disposable optics versus reusable optics is really driven primarily by economics. We can get into some of the details a little bit later. Economics is really a big driver of selection and another has to do with safety and cross-contamination of devices.
Ultimately, what we’re really talking about here are a classification of optical devices and how they’re used, whether they’re reused repeatedly or they’re used one time and discarded or somewhere in between.
Q: When we say, devices and what we’re looking at, let’s define that first before we actually hop into reusable versus the different options available out there, from a manufacturing standpoint.
A: Yes, good idea because it is a really broad topic. In general, you can categorize this as medical devices being reusable or disposable but I’m really focused on the visualization and imaging side of things. Really medical cameras, endoscopic devices, anything that’s used to look on, at, or in the body. Quite often, they’re used in conjunction with therapeutic devices.
At Lighthouse, our entire mission is to create, design, and manufacture imaging devices that are generally accessories or complementary to our customers’ own medical devices. That’s really what we’re talking about here, is the imaging and therapeutic side of medical devices.
Q: Right, and we’re not just talking about flashlights either. These are high tech and in some cases, invasive ways to look inside the body. It’s actually becoming an increasingly more important piece of the consideration as new devices come out as technology improves, and the evolution of devices and sensors really change the medical space, right?
A: That’s absolutely correct. There’s a lot of different drivers in when do you use a disposable or not. I think some of those become a little bit more obvious when you understand the differentiation between a reusable and a disposable device.
Q: That differentiation is actually really important. When we’re initially meeting with clients, sometimes you have to define that, right?
A: Yes, absolutely. I think it’s quite important. Generally, our clients are medical device manufacturers, and they will typically understand the ins and outs, but not always. It’s often important to have that conversation up front, so that we’re speaking the same language, because we find that sometimes different specific parts of the industry gets segmented or siloed in how they describe things, name things, and use things. You’re absolutely right.
Q: I think this is really fascinating because there’s so many factors that go into what a client will actually end up using. Obviously, use cases, how invasive the procedure could be, and those types of things, right? Why don’t we give an overview of how you evaluate reusable and disposable options for your clients, and what are the check-boxes that they have to hit in order to choose one or the other?
A: Actually, in order to answer that question, maybe just some very high-level definitions of what we’re talking about when we say reusable or disposable, and I think that may help to answer some of the more detailed questions. Classically, most medical devices have been reusable. What we mean by that is, is a device that’s either used for therapeutic or diagnostic applications that is used multiple times on multiple patients and has some method of cleaning, disinfection, and or sterilization in between.
You can think of this as, let’s say, like a saw that may be used for bones. That’s a pretty expensive device and you’re not going to want to throw that away every time. Generally, it’s a big piece of metal, once you use it, it’s pretty straightforward to scrub it, clean it, disinfect it, and then sterilize it through either autoclave or vaporized hydrogen peroxide, or a few other methods.
Q: Can I just say that that is a super visceral image? Just the thought of a saw going into my body to cut my bones, the good thing is that we’re out for that, right?
A: Right. The world of orthopedics is that fairly medieval in how it’s applied. If we try to focus this in a little bit more on Lighthouse and the work we do, you could think about a standard endoscope that has been around for decades in which there’s a whole series of glass lenses, is inside of a tube, and then some glass fibers that are used for illumination and it’s a very expensive piece of equipment, it may be thousands of dollars if not tens of thousands of dollars.
The same is also true for flexible scopes that are used in gastroenterology, colonoscopies, those for gastrology, those kinds of applications. They’re long, have a lot of material, a lot of tiny parts, and moving parts, and very expensive. Generally, hospitals and doctors want to reuse those. They’re not going to use a $10,000 device once and get rid of it. That kind of equipment really is the baseline and the foundation of how medicine has worked really over the last century.
As we started to understand the anesthetics, the anesthesia, and the ability to reprocess and sterilize things, we’ve really been able to capitalize on repeated use of equipment for cost-effectiveness. We often refer to this kind of equipment as CapEx, or capital expenditure. What we mean by that is, it’s a valuable piece of equipment that gets used repeatedly and will generally have a long life of many years. That’s a broad overview of what a reusable device might be.
Let’s look at the other end of the spectrum, which is a disposable device. On the inside of the industry, we tend to use the word disposable a lot, but it’s also synonymous with single-use. We also use single-use more in literature and marketing material because has a better connotation, disposable basically directly infers that there is some sort of garbage or waste at the end of the usage.
A disposable is just that. It’s a device that is used one time on one patient and then it’s discarded and never used again. As you can imagine, it’s a completely different working paradigm than a device that gets used over, and over, and over.
Q: Going back to the reusable or single-use, we can change that vernacular right here, because for some clients, with reusable, the one thing to point out sometimes when you’re thinking about medical devices is, how safe and how clean it is. We actually here at Lighthouse take all of that into account as well. When we’re developing solutions with our clients, we take into account what if we’re going to add illumination to it in some capacity, how is it taken care?
A: There’s certainly a different approach to developing and manufacturing a reusable versus a single-use device. Again, it’s largely driven by a cost, but it’s also driven by the used case and the need to clean or not clean and sterilize a device.
Q: I just like to point that out because when we go through these types of audits and discoveries with clients, it’s really important that they understand that just because it’s been created, doesn’t mean that’s the end. We have to help that. Then with single-use, their methodologies, and protocols, they are necessary to follow to remove that as well. Those are all taken into consideration when we work with the clients and help educate them on what those policies and procedures are as well.
A: Absolutely.
Q: When we say, CapEx or Capital Expenditures and reference them in the device setting. What do you mean by that.
A: If I’m using endoscopy as an example, a world that we live in every day, there really can be two pieces to it. There is the device itself, which is just to be very general, the camera or the endoscope side of things that actually goes inside of the patient. If that’s a reusable device, typically it falls into a category of capital expenditure.
There’s also a back end or a processing side of things that is typically even more expensive than the device itself. A lot of times you’ll find an endoscopic tower in the same facility where the endoscope is used. That’s doing all the video processing, providing the light and the recording and displaying. There’s usually a few other functions that also get thrown into the cart as well.
That can easily be a $1,000 or more or less obviously, but can very easily be a $100,000 for that tower of equipment which actually segues into an interesting paradigm that we see gaining a lot of traction on the market. We referred to this as a hybrid system or a hybrid single-use system, where you still have that capital expenditure backend processing, but the device itself is as a single-use device.
You would have ideally a very low-cost portion of the device that gets thrown away after each use and then you reuse the really expensive part. What’s interesting though that we find with the level of customization that a Lighthouse can do, our capital expenditure equipment, the backend processing is rarely on the same order of magnitude of cost as a traditional large tower system.
Typically the devices, the processing side of the devices that we’re working on are much smaller and lower cost. They can be a tabletop mount, cart mount or they could even be handheld and battery powered. They come at a lower overhead than a traditional endoscopic system.
Q: We’re talking about the use cases and the reasons for being reusable or single-use devices. You go through different options of illumination in your medical devices, It’s a really fascinating topic because it applies or can apply to so many different procedures and so many types or classes of medical devices. Is that correct?
A: It’s absolutely correct. We’re at an inflection point in the world of medical devices right now and particularly imaging and camera type devices where a lot of equipment is being considered for application of single-use devices. We’re starting to see that transition right now. Really driven by cost parameters as well as safety and cross-contamination risk factors.
Q: Do you think that one of those driving factors is the improvement of technology, but at the same time the reduction in cost because the technology continues to improve?
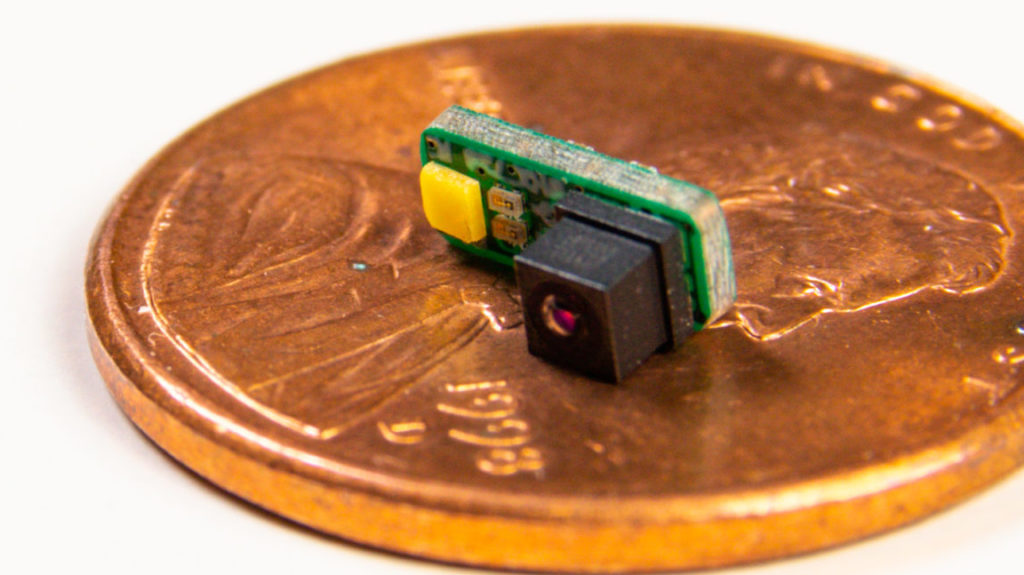
A: Yes. That’s absolutely true. It is largely driven by the technology on the cost and performance side of things. Largely at least in our world, it’s driven by a reduction in the size of image sensors. 10 years ago, the smallest image sensor you could get was in the order of a couple millimeters by a couple millimeters, which was tiny at that point in time. We can now get image sensors that are half a millimeter by a half a millimeter in size and with usable resolution and video performance to apply to a lot of different applications.
Q: Do you see that imaging is now being applied to procedures that 10 years ago it wouldn’t even be considered?
A: Absolutely. We see this quite regularly. In one area that we’re heavily involved is, laryngoscopy and airway management. This would be a scenario where you might want to be putting a breathing tube into a patient. Historically, that was done basically by sticking a stiff wire down somebody’s throat and using that wire to hold the tongue and other things.
You guide the tube in and then advance in the laryngoscope that has a flat blade on it. Then, eventually, that transitioned into adding cameras and visualization. It’s been a progression of minimally effective technique, but still useful to now being guided by imagery and even by some computer vision systems that basically tell the user or the operator where to go rather than relying on decades of experience on exactly how to do it.
Q: The ability to store that data and then compare objectively across different patients and share these practices. It’s only improving everything that we can do. Are there FDA requirements now that have muddied the waters at all? Are there any hindrances to people continuing to innovate and try imaging on procedures that had never been done before?
A: The imaging side itself depending on whether it’s therapeutic or diagnostics does have some regulatory element. One of the things that we see in regards to disposable versus reusable devices is driven by the cleanliness of a product. There had been recent cases of severe illnesses and even death based upon cross contamination when a device gets used on one patient.
It gets cleaned and supposedly sterilized, but the sterilization process wasn’t fully effective, it gets used on another patient and now infectious diseases from patient A are now transferred to patient B. It’s a very serious scenario. There’s health liabilities and risk, as well as financial considerations for both medical device manufacturers and hospitals and doctors.
This has really pushed a lot of interest in disposable devices based upon the complexity of cleaning reusable devices that are being cracked down on by the FDA at this point of time because of some of these recent instances.
Q: Has that meant going back to the drawing board with the existing clients or has that lead to new solutions that you’ve just never had in the past?
A: Luckily, Lighthouse has never been involved with the devices that have caused cross-contamination. Recently, I guess these have occurred by very large medical manufacturers. Generally, we’re working on various specific devices and various specific application. We’re thinking through the process very thoroughly. Ultimately, it is up to our client and the final user to make sure that something is cleaned appropriately.
The device has to be designed and instructions have to be provided for how to effectively do so. What we see is as we start adding visualization to devices that didn’t have it before, typically, those devices already have methods for cleaning. It’s our responsibility then to design in the physical geometries that allow cleaning as well as the ability of the device itself to survive on the cleaning and sterilization.
Q: What’s the best way for clients to start making that evaluation and specific considerations to make as they start to enter the market or want to enter the market with a solution that is going to change their world?
A: First and foremost, that decision should be driven by efficacy and safety, but obviously, economics become a very big player as well. If a device is just not economically viable, it won’t get developed. Typically, that’s one of the first hurdles is making sure that the economics of a single use system makes sense. Otherwise, either that device wouldn’t be developed or a different approach would be taken.
Q: Right and how can people get in touch with you to start this process?
A: Yes, absolutely. Well, I would recommend going to our website, www.lighthouseoptics.com. We have information as well as links to send messages to anyone on the team. We are very prompt in responding and it offers a great customized and personal service.